Every day in the U.S., 10,000 people turn 65, and the number of older adults will more than double over the next several decades to top 88 million people and represent over 20 percent of the population by 2050. The rapid pace of change creates an opportunity and an imperative for both the public and private sector to harness the potential of the growing segment of society and to ensure the welfare of older Americans.
Americans’ increased longevity, coupled with the need to finance a growing share of their own care, are major factors driving older adults to delay retirement and remain in the labor force. While the U.S. labor force is expected to grow at just 0.5 percent over the next decade, adults over age 65 represent the fastest-growing segment. Recognizing this productive potential and the need to retain skilled workers and transfer institutional knowledge, companies and other employers are beginning to introduce phased-retirement and part-time work opportunities.
High and increasing costs of healthcare present significant challenges to older Americans who are increasingly aging in place. While the Americans with Disability Act has made the U.S. a leader in accessibility, the rapid pace of aging is challenging the public, private, and non-profit sectors to effectively address the social services and care needs of older adults across urban and rural areas. As leaders in innovation, corporations and start-ups are developing technologies and age-focused apps that could significantly enhance the safety, security, and well-being of older Americans increasingly aging in place.
Every day in the United States, 10,000 people turn 65, and the number of older adults will more than double over the next several decades and represent over 20 percent of the population by 2050.
Source: UN Population Division

Community Social Infrastructure
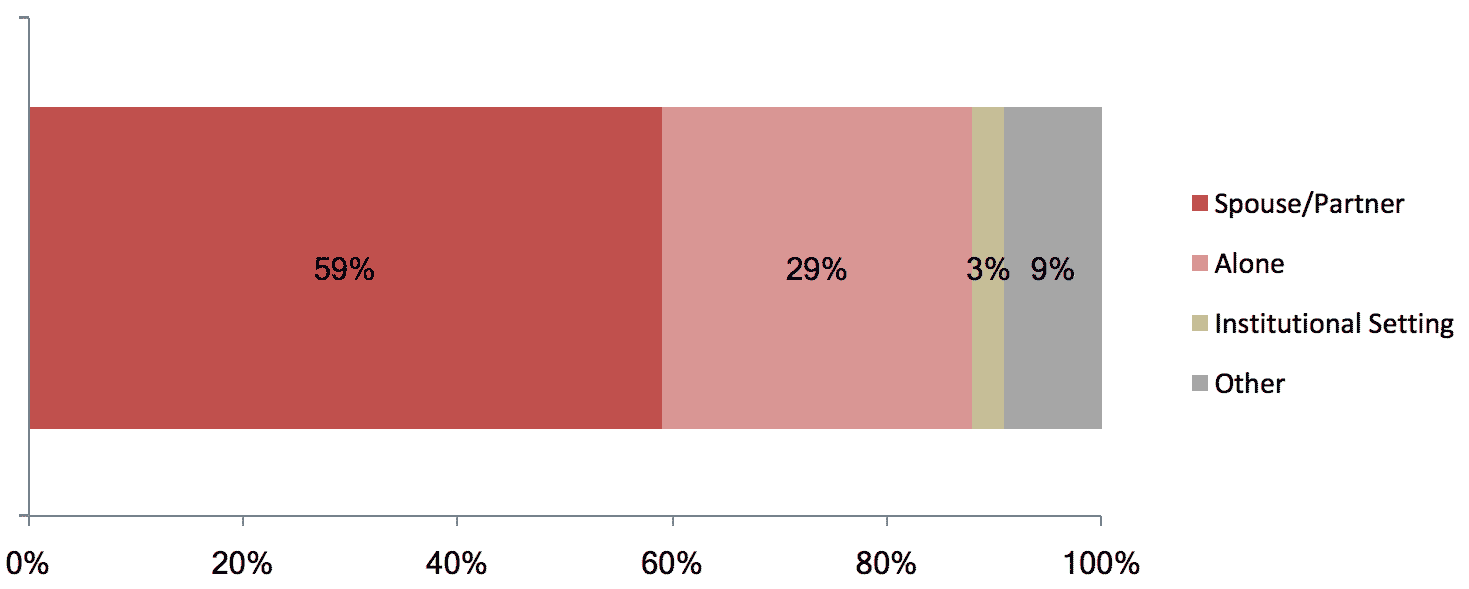
The relatively independent nature of American culture and the tendency for older adults to live alone or with their spouse and away from their children put older adults in the U.S. particularly at risk of social isolation. Limited transportation options and the lack of affordable housing have been identified as leading issues inhibiting connectedness and social interaction. A network of public, private, and community-based service organizations are striving to provide meal delivery and a range of in-home services in an effort to meet the growing and varied needs of the older U.S. population, which is increasingly aging in place.
Millions of older Americans suffer from persistent loneliness – 32 percent of people ages 60 through 69 and 25 percent of those age 70 and older reportedly feel lonely.
Source: U.S. Department of Health & Human Services
Living Arrangements of Adults 65+ in 2016
Federal and state government support is channeled, to a large extent, through community organizations, which play a vital role in helping older adults to live independently and age in place. However, funds have not kept pace with the needs of the growing aging population. In light of tenuous funding, organizations supporting the aging are seeking supplemental resources for survival.
The federal funds allocation rose minimally from USD 1.80 billion in FY 2004 to USD 1.88 billion in FY 2014, while the population of people ages 65 and older grew by nearly 30 percent over the same period.
National Association of Area Agencies on Aging (n4a) and Meals on Wheels America
Recognizing the myriad risks associated with loneliness and social isolation, organizations such as the National Association of Area Agencies on Aging (n4a), which has 622 area agencies that provide a range of services such as meals, rides, home visits and care services, seek to mitigate the adverse impacts of isolation. One long-lasting and effective program is Meals on Wheels America, which runs through a network of 5,000 independently run local programs delivering daily meals to isolated and vulnerable older adults.
Productive Opportunity
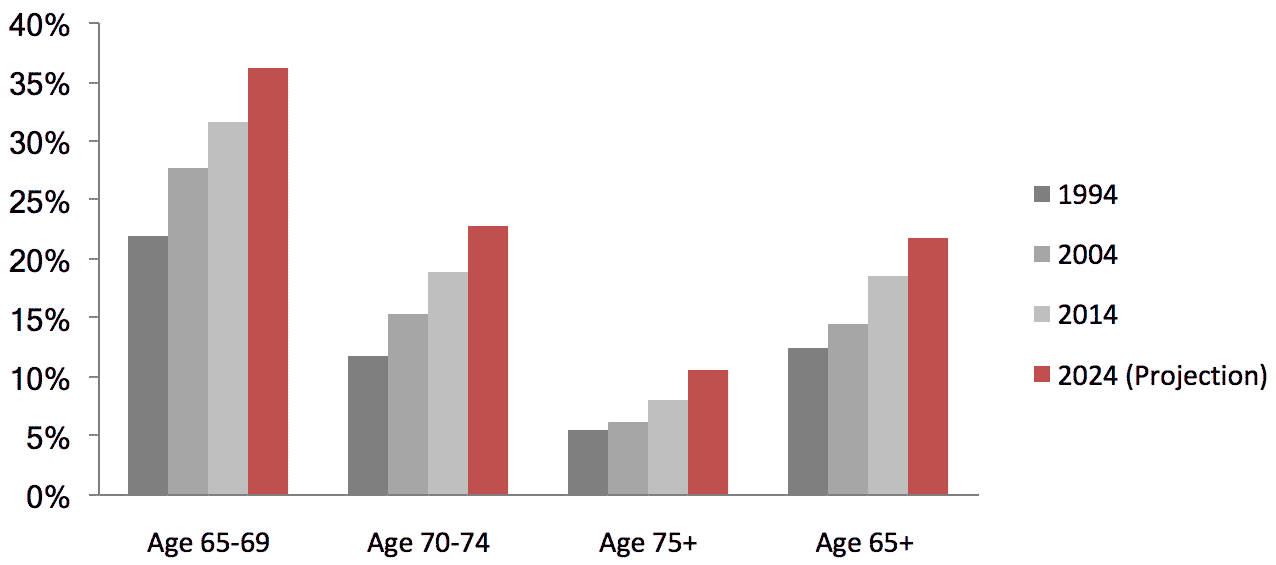
Older Americans’ labor force participation rate has increased dramatically over the past several decades and is up by more than 50 percent over the period of 2000 through 2017, with participation by older women growing over 70 percent during that period. The labor force participation rate for both men and women is expected to grow further to reach 21.7 percent by 2024. The upward trend is a result of converging factors, including acute economic shocks, which adversely impacted retirement accounts, a shift toward employee-driven benefit plans, and an increasing number of older adults electing to remain in the labor force. As Americans are living longer lives and need greater economic security, a growing number are seeking to stay at or return to work.
Older Americans tend to be more active in the labor market than counterparts in most OECD countries.
The labor force participation rate of people age 65 and older in the U.S. was 18.9 percent as of 2015, more than one-third higher than the OECD average.
U.S. Labor Participation Rate by Age Group
While Americans are working longer, a looming wave of retiring baby boomers and an impending skills gap have policymakers and management across economic sectors looking at ways to phase retirement, extend productive potential, and pass on institutional knowledge to the next generation. However, age discrimination and a lack of familiarity with new technology, among other issues, remain barriers to employment.
It is estimated that 2.7 million jobs are likely to be needed due to retirement within the existing labor force, while more than 700,000 new jobs will be created from economic growth.
“Minor tweaks could make the social security system more flexible and create incentives for seniors to work longer. For example, if people want to stop working for a little while to obtain training they shouldn’t lose credits.”
– Jim Emerman, Executive Vice President, Encore

Technological Engagement
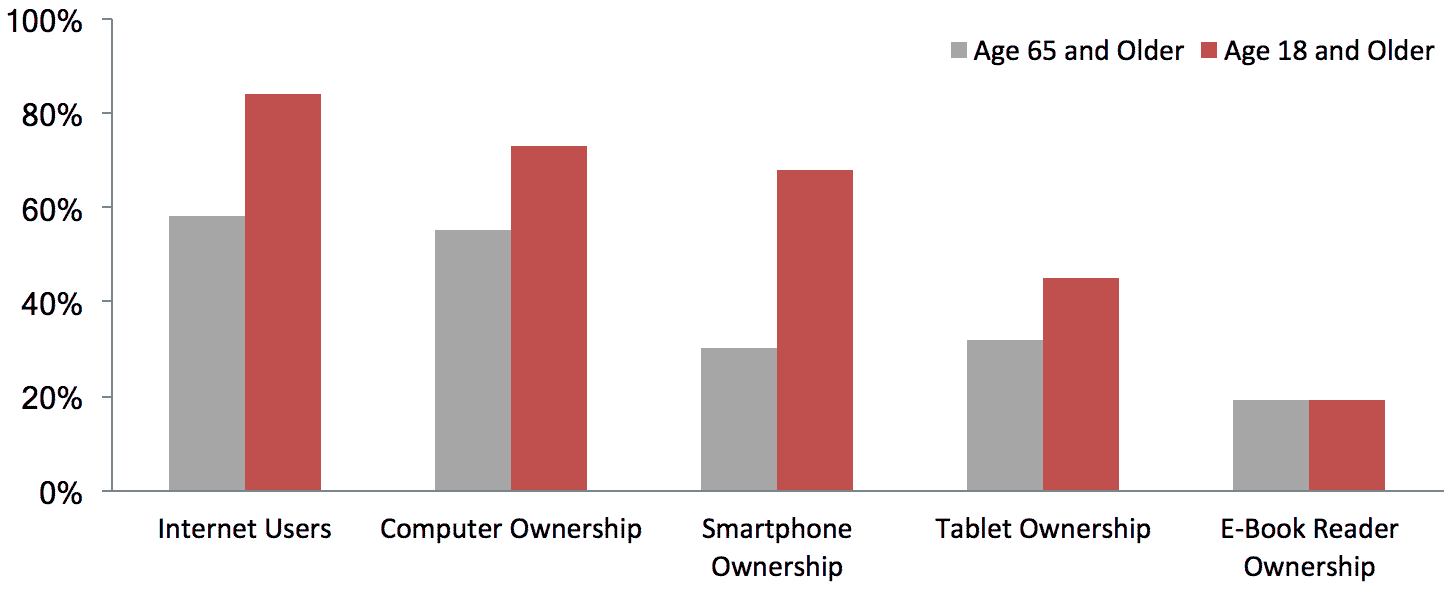
The U.S. is a leader in digital technology penetration, with an increase in technology utilization by older Americans who are seeking greater social connection, assistance with personal tasks, support in the workplace, and health and home care. The Internet-penetration gap in the U.S. is among the smallest within OECD countries. However, Internet access and the expansion of broadband services, particularly into rural areas, has been and continues to be critical to service delivery. Expanded coverage will be key to enabling the proliferation and penetration of assistance technologies. Senior centers and social service agencies are integrating programs and classes designed to enhance older adults’ digital competency and fluency. In some select cases, centers are exclusively dedicated to facilitating older adults’ digital technology adoption.
Adoption of Digital Technology As of 2015
Percentage of Population of Each Group
High-Tech Innovation for the Aging – Hot Topic at SXSW
In an effort to capitalize on the demographic shift and the associated market opportunities, a range of start-up companies are developing solutions specifically targeting the aging population. New tech-based solutions and applications that specifically target the aging were on display at the 2017 South by Southwest conference showcasing cutting-edge technologies, with companies launching a range of safety, security, and communications tools for older adults. However, the vast majority of older adults still need assistance with understanding and utilizing these technologies, and a range of service organizations are developing tech-related education and training programs to help older adults effectively leverage these new technologies to enhance their quality of life.
Healthcare & Wellness
While older Americans’ lifespans have improved over the past decade, they remain below the average for high-income countries. A range of factors are contributing to America’s relatively poor and deteriorating health outcomes, including education, income, job security, food insecurity, and the social safety net. Given the high cost and growing healthcare demand, there remains an acute need for improved healthcare coverage. While federal health insurance programs for older adults do exist, they only cover a portion of costs. Demand for healthcare and long-term-care services has been increasing and is expected to rise rapidly in the coming decades. Medicaid is the only program that provides financial support for long-term care, and future funding is tenuous.
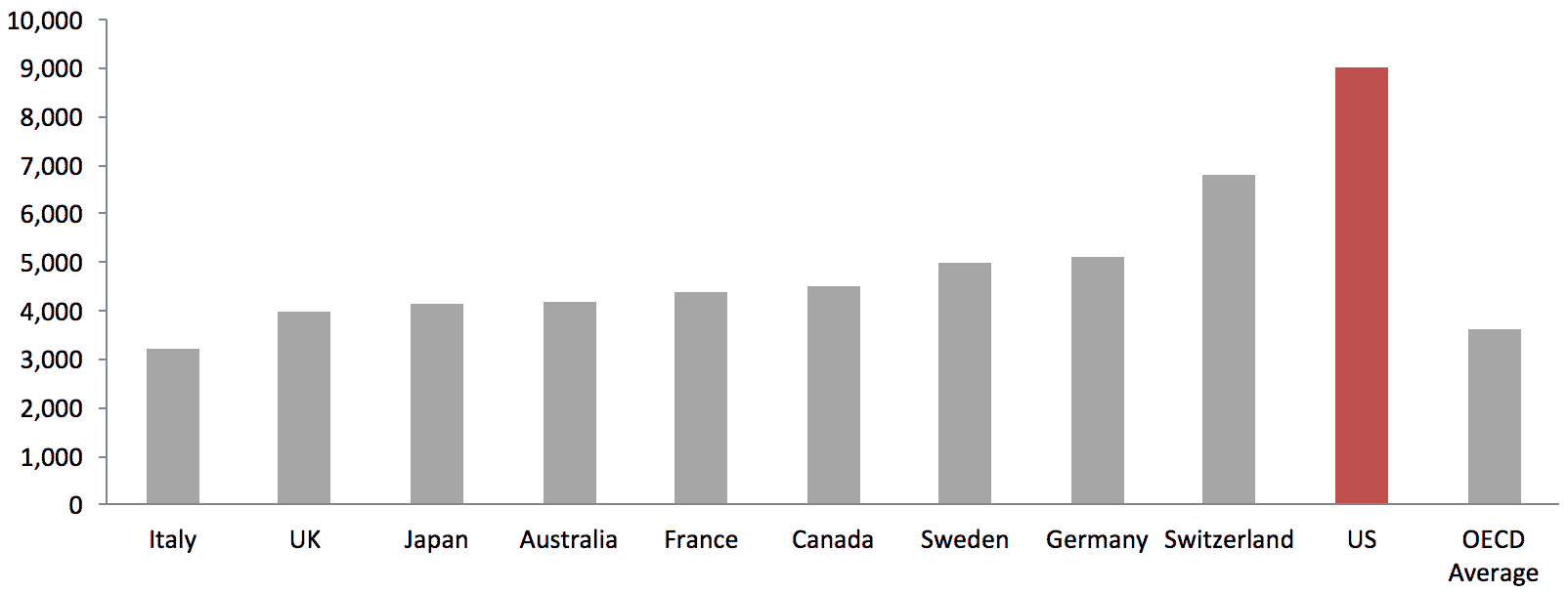
U.S. per capita healthcare spending is the highest in the world, more than twice the average of other developed countries. Yet, Americans have lower life expectancies and higher rates of chronic illnesses than OECD counterparts.
Source: OECD Statistics, 2016
Healthcare Costs Per Capita (USD)
Given the cost of facilities and the loss of independence, among other factors, older Americans tend to prefer to age in place. Demand for home health care support is increasing and is expected to be one of the fastest-growing sectors in terms of job creation.
According to the Bureau of Labor Statistics, 1.3 million new jobs in the home healthcare field are expected to be created through 2020 – a 69 percent growth rate, compared with an average 14 percent across other sectors.
The National Institutes of Health (NIH) and the Go4Life Campaign are Turning Attention on Prevention
The NIH and the Go4Life Campaign are fostering the integration of physical exercise into the lives of older adults. As of 2015, the Go4Life campaign had developed more than 250 public and private partners, many of whom host Go4Life monthly activities – including endurance, strength, balance, flexibility exercises, and promotion of healthy lifestyles. Not only do these types of public-private partnerships expand the reach of services, they are not completely reliant on government dollars and are less vulnerable to funding cuts.